Abstract
Immunotherapy revolutionized treatment options in cancer, yet the mechanisms underlying resistance in many patients remain poorly understood. Cellular proteasomes have been implicated in modulating antitumor immunity by regulating antigen processing, antigen presentation, inflammatory signaling and immune cell activation. However, whether and how proteasome complex heterogeneity may affect tumor progression and the response to immunotherapy has not been systematically examined. Here, we show that proteasome complex composition varies substantially across cancers and impacts tumor–immune interactions and the tumor microenvironment. Through profiling of the degradation landscape of patient-derived non-small-cell lung carcinoma samples, we find that the proteasome regulator PSME4 is upregulated in tumors, alters proteasome activity, attenuates presented antigenic diversity and associates with lack of response to immunotherapy. Collectively, our approach affords a paradigm by which proteasome composition heterogeneity and function should be examined across cancer types and targeted in the context of precision oncology.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
RNA-seq data that support the findings of this study have been deposited in the Gene Expression Omnibus (GEO) under accession code GSE201460. scRNA-seq data have been deposited to the ArrayExpress database at EMBL-EBI (www.ebi.ac.uk/arrayexpress) under accession code E-MTAB-10745. Mass spectrometry data (list in Supplementary Table 3) have been deposited to the ProteomeXchange Consortium via the PRIDE84 partner repository with the primary accession codes PXD019573, PXD028364 and PXD037365 (https://www.ebi.ac.uk/pride/). Previously published data from ICB-treated cohorts that were re-analyzed here are available under accession codes EGAS00001002556, EGAS00001002928, GSE78220 and GSE91061. Human PANCAN transcriptomics data were derived from the TCGA Research Network: http://cancergenome.nih.gov/, and CPTAC: https://proteomics.cancer.gov/data-portal. Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding authors on reasonable request.
Code availability
Custom code used in this manuscript is available at https://github.com/merbllab/PSME4_NatCancer.
References
Johnson, D. B., Nebhan, C. A., Moslehi, J. J. & Balko, J. M. Immune-checkpoint inhibitors: long-term implications of toxicity. Nat. Rev. Clin. Oncol. 19, 254–267 (2022).
Rock, K. L., Reits, E. & Neefjes, J. Present yourself! By MHC class I and MHC class II molecules. Trends Immunol. 37, 724–737 (2016).
Rousseau, A. & Bertolotti, A. Regulation of proteasome assembly and activity in health and disease. Nat. Rev. Mol. Cell Biol. 19, 697–712 (2018).
Salzmann, U. et al. Mutational analysis of subunit iβ2 (MECL-1) demonstrates conservation of cleavage specificity between yeast and mammalian proteasomes. FEBS Lett. 454, 11–15 (1999).
Driscoll, J., Brown, M. G., Finley, D. & Monaco, J. J. MHC-linked LMP gene products specifically alter peptidase activities of the proteasome. Nature 365, 262–264 (1993).
Gaczynska, M., Rock, K. L. & Goldberg, A. L. γ-Interferon and expression of MHC genes regulate peptide hydrolysis by proteasomes. Nature 365, 264–267 (1993).
Winter, M. B. et al. Immunoproteasome functions explained by divergence in cleavage specificity and regulation. eLife 6, e27364 (2017).
Chong, C. et al. High-throughput and sensitive immunopeptidomics platform reveals profound interferonγ-mediated remodeling of the human leukocyte antigen (HLA) ligandome. Mol. Cell. Proteomics 17, 533–548 (2018).
Javitt, A. et al. Pro-inflammatory cytokines alter the immunopeptidome landscape by modulation of HLA-B expression. Front. Immunol. 10, 141 (2019).
Riaz, N. et al. Tumor and microenvironment evolution during immunotherapy with nivolumab. Cell 171, 934–949.e16 (2017).
Tripathi, S. C. et al. Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome. Proc. Natl Acad. Sci. USA 113, E1555–E1564 (2016).
Kalaora, S. et al. Immunoproteasome expression is associated with better prognosis and response to checkpoint therapies in melanoma. Nat. Commun. 11, 896 (2020).
Blickwedehl, J. et al. The proteasome activator PA200 regulates tumor cell responsiveness to glutamine and resistance to ionizing radiation. Mol. Cancer Res. 10, 937–944 (2012).
Ustrell, V., Hoffman, L., Pratt, G. & Rechsteiner, M. Pa200, a nuclear proteasome activator involved in DNA repair. EMBO J. 21, 3516–3525 (2002).
Welk, V. et al. Inhibition of proteasome activity induces formation of alternative proteasome complexes. J. Biol. Chem. 291, 13147–13159 (2016).
Qian, M.-X. et al. Acetylation-mediated proteasomal degradation of core histones during DNA repair and spermatogenesis. Cell 153, 1012–1024 (2013).
Fabre, B. et al. Label-free quantitative proteomics reveals the dynamics of proteasome complexes composition and stoichiometry in a wide range of human cell lines. J. Proteome Res. 13, 3027–3037 (2014).
Toste Rêgo, A. & da Fonseca, P. C. A. Characterization of fully recombinant human 20S and 20S-PA200 proteasome complexes. Mol. Cell 76, 138–147.e5 (2019).
Tsvetkov, P. et al. Suppression of 19S proteasome subunits marks emergence of an altered cell state in diverse cancers. Proc. Natl Acad. Sci. USA 114, 382–387 (2017).
Tanahashi, N. et al. Molecular properties of the proteasome activator PA28 family proteins and γ-interferon regulation. Genes Cells 2, 195–211 (1997).
Sánchez-Martín, D. et al. Proteasome activator complex PA28 identified as an accessible target in prostate cancer by in vivo selection of human antibodies. Proc. Natl Acad. Sci. USA 110, 13791–13796 (2013).
Kisselev, A. F. F., Akopian, T. N. N., Woo, K. M. M. & Goldberg, A. L. L. The sizes of peptides generated from protein by mammalian 26 and 20 S proteasomes. Implications for understanding the degradative mechanism and antigen presentation. J. Biol. Chem. 274, 3363–3371 (1999).
Ruschak, A. M. & Kay, L. E. Proteasome allostery as a population shift between interchanging conformers. Proc. Natl Acad. Sci. USA 109, E3454–E3462 (2012).
Yamano, T. et al. Allele-selective effect of PA28 in MHC class I antigen processing. J. Immunol. 181, 1655–1664 (2008).
de Graaf, N. et al. PA28 and the proteasome immunosubunits play a central and independent role in the production of MHC class I-binding peptides in vivo. Eur. J. Immunol. 41, 926–935 (2011).
Murata, S., Takahama, Y., Kasahara, M. & Tanaka, K. The immunoproteasome and thymoproteasome: functions, evolution and human disease. Nat. Immunol. 19, 923–931 (2018).
Dick, T. P. et al. Coordinated dual cleavages induced by the proteasome regulator PA28 lead to dominant MHC ligands. Cell 86, 253–262 (1996).
Wolf-Levy, H. et al. Revealing the cellular degradome by mass spectrometry analysis of proteasome-cleaved peptides. Nat. Biotechnol. 36, 1110–1116 (2018).
Javitt, A. & Merbl, Y. Global views of proteasome-mediated degradation by mass spectrometry. Expert Rev. Proteomics https://doi.org/10.1080/14789450.2019.1651979 (2019).
Litchfield, K. et al. Meta-analysis of tumor- and T cell-intrinsic mechanisms of sensitization to checkpoint inhibition. Cell 184, 596–614.e14 (2021).
Kim, J. Y., Choi, J. K. & Jung, H. Genome-wide methylation patterns predict clinical benefit of immunotherapy in lung cancer. Clin. Epigenetics 12, 1–10 (2020).
Gillette, M. A. et al. Proteogenomic characterization reveals therapeutic vulnerabilities in lung adenocarcinoma. Cell 182, 200–225.e35 (2020).
Kahana, C. & Reiss, Y. Cell-free assay for ubiquitin-independent proteasomal protein degradation. Methods Mol. Biol. 301, 83–96 (2005).
Pishesha, N., Harmand, T. J. & Ploegh, H. L. A guide to antigen processing and presentation. Nat. Rev. Immunol. 22, 751–764 (2022).
Lavin, Y., Kobayashi, S., Leader, A. & Rahman, A. Innate immune landscape in early lung adenocarcinoma by paired single-cell analyses. Cell 169, 750–757.e15 (2017).
Maier, B. et al. A conserved dendritic-cell regulatory program limits antitumour immunity. Nature 580, 257–262 (2020).
Li, S., Wu, J., Zhu, S., Liu, Y. J. & Chen, J. Disease-associated plasmacytoid dendritic cells. Front. Immunol. https://doi.org/10.3389/fimmu.2017.01268 (2017).
Morozov, A. V. & Karpov, V. L. Proteasomes and several aspects of their heterogeneity relevant to cancer. Front. Oncol. 9, 761 (2019).
Cantin, A. M. & Richter, M. V. Cigarette smoke-induced proteostasis imbalance in obstructive lung diseases. Curr. Mol. Med. 12, 836–849 (2012).
Kammerl, I. E. et al. Dissecting the molecular effects of cigarette smoke on proteasome function. J. Proteomics 193, 1–9 (2019).
Srinivas, U. S., Tan, B. W. Q., Vellayappan, B. A. & Jeyasekharan, A. D. ROS and the DNA damage response in cancer. Redox Biol. https://doi.org/10.1016/j.redox.2018.101084 (2019).
Young, J. H. et al. Computational discovery of pathway-level genetic vulnerabilities in non-small-cell lung cancer. Bioinformatics 32, 1373–1379 (2016).
Jiang, T.-X. et al. Proteasome activator PA200 maintains stability of histone marks during transcription and aging. Theranostics 11, 1458 (2021).
Wani, P. S., Rowland, M. A., Ondracek, A., Deeds, E. J. & Roelofs, J. Maturation of the proteasome core particle induces an affinity switch that controls regulatory particle association. Nat. Commun. 6, 6384 (2015).
Marques, A. J., Glanemann, C., Ramos, P. C. & Dohmen, R. J. The C-terminal extension of the β7 subunit and activator complexes stabilize nascent 20 S proteasomes and promote their maturation. J. Biol. Chem. 282, 34869–34876 (2007).
Boulpicante, M. et al. Tumors escape immunosurveillance by overexpressing the proteasome activator PSME3. Oncoimmunology 9, 1761205 (2020).
Sahu, I. & Glickman, M. H. Structural insights into substrate recognition and processing by the 20S proteasome. Biomolecules 11, 1–15 (2021).
Huang, L., Marvin, J. M., Tatsis, N. & Eisenlohr, L. C. Cutting edge: selective role of ubiquitin in MHC class I antigen presentation. J. Immunol. 186, 1904–1908 (2011).
Wei, J. et al. Varied role of ubiquitylation in generating MHC class I peptide ligands. J. Immunol. 198, 3835 (2017).
Abi Habib, J., Lesenfants, J., Vigneron, N. & Van den Eynde, B. J. Functional differences between proteasome subtypes. Cells 11, 421 (2022).
van Endert, P. Intracellular recycling and cross-presentation by MHC class I molecules. Immunol. Rev. 272, 80–96 (2016).
Buneeva, O. A. & Medvedev, A. E. Ubiquitin-independent degradation of proteins in proteasomes. Biochem. (Mosc.) Suppl. B Biomed. Chem. 12, 203–219 (2018).
Mamrosh, J. L. et al. A systematic interrogation of MHC class I peptide presentation identifies constitutive and compensatory protein degradation pathways. Preprint at bioRxiv https://doi.org/10.1101/2021.10.07.463289 (2022).
Yewdell, J. W., Dersh, D. & Fåhraeus, R. Peptide channeling: the key to MHC class I immunosurveillance? Trends Cell Biol. 29, 929–939 (2019).
Blum, J. S., Wearsch, P. A. & Cresswell, P. Pathways of antigen processing. Annu. Rev. Immunol. 31, 443–473 (2013).
Lev, A. et al. Compartmentalized MHC class I antigen processing enhances immunosurveillance by circumventing the law of mass action. Proc. Natl Acad. Sci. USA 107, 6964–6969 (2010).
Yewdell, J. W., Norbury, C. C. & Bennink, J. R. Mechanisms of exogenous antigen presentation by MHC class I molecules in vitro and in vivo: implications for generating CD8+ T cell responses to infectious agents, tumors, transplants, and vaccines. Adv. Immunol. 73, 1–77 (1999).
Harel, M. et al. Proteomics of melanoma response to immunotherapy reveals mitochondrial dependence. Cell 179, 236–250.e18 (2019).
Spits, M. & Neefjes, J. Immunoproteasomes and immunotherapy—a smoking gun for lung cancer? J. Thorac. Dis. 8, E558–E563 (2016).
Boshuizen, J. & Peeper, D. S. Rational cancer treatment combinations: an urgent clinical need. Mol. Cell 78, 1002–1018 (2020).
Pfirschke, C. et al. Immunogenic chemotherapy sensitizes tumors to checkpoint blockade therapy. Immunity 44, 343–354 (2016).
Mariathasan, S. et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554, 544–548 (2018).
McDermott, D. F. et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat. Med. 24, 749–757 (2018).
Snyder, A. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. New Engl. J. Med. 371, 2189–2199 (2014).
Hugo, W. et al. Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell 165, 35–44 (2016).
Van Allen, E. M. et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science 350, 207–211 (2015).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849 (2016).
Wickam, H. ggplot2: Elegant Graphics for Data Analysis (Springer-Verlag New York, 2016).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Trujillo, J. A., Sweis, R. F., Bao, R. & Luke, J. J. T cell-inflamed versus non-T cell-inflamed tumors: a conceptual framework for cancer immunotherapy drug development and combination therapy selection. Cancer Immunol. Res. 6, 990–1000 (2018).
Spranger, S., Bao, R. & Gajewski, T. F. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature 523, 231–235 (2015).
Uhlen, M. et al. A pathology atlas of the human cancer transcriptome. Science 357, eaan2507 (2017).
Thul, P. J. et al. A subcellular map of the human proteome. Science 356, 6340 (2017).
Uhlén, M. et al. Tissue-based map of the human proteome. Science 347, 6220 (2015).
Welk, V. et al. Proteasome activator PA200 regulates myofibroblast differentiation. Sci. Rep. 9, 1–11 (2019).
Klotz, L. et al. Comprehensive clinical profiling of the Gauting locoregional lung adenocarcinoma donors. Cancer Med. 8, 1486–1499 (2019).
Kohen, R. et al. UTAP: User-friendly Transcriptome Analysis Pipeline. BMC Bioinf. 20, 1–7 (2019).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177, 1888–1902.e21 (2019).
Grün, D. et al. Single-cell messenger RNA sequencing reveals rare intestinal cell types. Nature 525, 251–255 (2015).
Maier, B. et al. A conserved dendritic-cell regulatory program limits antitumour immunity. Nature 580, 257–262 (2020).
Heng, T. S. P. et al. The immunological genome project: networks of gene expression in immune cells. Nat. Immunol. 9, 1091–1094 (2008).
Raudvere, U. et al. G:Profiler: a web server for functional enrichment analysis and conversions of gene lists (2019 update). Nucleic Acids Res. 47, W191–W198 (2019).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Vizcaíno, J. A. et al. 2016 update of the PRIDE database and its related tools. Nucleic Acids Res. 44, D447–D456 (2016).
Acknowledgements
We thank the members of the Merbl lab as well as B. Dassa and A. Erez for discussion and critical reading of the manuscript. We thank A. Zippelius for KP1.9 cells. Y.M. is supported by the European Research Council (ERC; grant agreement no. 677748 (StG) and no. 101045613 (CoG)) under the European Union’s Horizon 2020 research and innovation program; the I-CORE Program of the Planning and Budgeting Committee and the Israel Science Foundation (grant no. 1775/12); the Cancer Research Institute/Israel Cancer Research Fund CLIP Grant (no. CRI4351); the Melanoma Research Alliance award (https://doi.org/10.48050/pc.gr.143730; Pilot Award program, grant agreement 826874); and the Abisch—Frenkel Foundation for the Promotion of Life Sciences (grant no. 18/WIS3). M.D.S. is supported by a Marie Sklodowska-Curie Individual Fellowship (Horizon 2020 grant no. GAP-845066).
Author information
Authors and Affiliations
Contributions
A.J., M.D.S. and Y.M. conceived, designed and interpreted experiments and wrote the manuscript. A.E.-L. and S.M. provided feedback on the manuscript. M.D.S., A.U., H.W.-L. and A.E.-L. performed proteomics preparation and M.D.S. performed the in vitro work. M.P.K., I.J.C. and L.R. performed the in vivo and immunofluorescence experiments. A.A.K., M.P.K. and A.J. performed and analyzed the scRNA-seq experiments. M.D.S. and D.S. performed the bulk RNA-seq experiments. A.J. and K.L. analyzed the ICI cohort. I. Kramer, E.B.-D. and O.Z. conducted the immunohistochemistry experiments. V.N., E.S.-P., M.L. and I. Koch analyzed the German patient cohort. A.K. managed the NSCLC Israeli cohort. M.A. and M.D.S. performed immunopeptidomics and A.J. analyzed the data. Y.L. performed mass spectrometry. A.T.R. and P.C.A.D.F. purified recombinant PSME4. M.D.S. performed all other cellular and biochemical assays. A.J. performed all other bioinformatics. J.B., Y.S., E.E., N.F., C.S., S.M. and Y.M. funded and supervised the work of respective group members and Y.M. supervised the study. A.J. and M.D.S. contributed equally to the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Proteasome expression differs across tumor types.
a, Tumors were clustered by the expression of either the catalytic (PSMB5, PSMB6, PSMB7, PSMB8, PSMB9, PSMB10) or regulatory subunits (PSME1, PSME2, PSME3 and PSME4). We defined two clusters based on the catalytic cores that we defined as cProt – constitutitve proteasome and iProt – immunoproteasome based on the proteasome expression. Likewise, we defined 4 clusters based on the regulatory subunits that we defined as PSME4, PSME3, PSME1and2 and mixed based on the expression patterns. The graph shows the difference in the mean expression of each subunit for each cluster compared to the full dataset (color) as well as the significance of the difference between the mean and the background (circle size). b, The odds ratio of association with survival for the biomarker indicated for each of the cohorts used for the immunotherapy metaanalysis (n = 331 BLCA, 134 SKCM, 72 KIRC tumors). c, The spearman correlation between different biomarkers from the ICI1000 + study (n = 331 BLCA, 134 SKCM, 72 KIRC tumors). Circle size shows absolute correlation coefficient and asterisks indicate correlation significance. Precise p values are presented in source data.
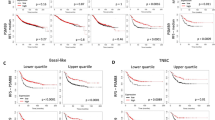
Extended Data Fig. 2 PSME4 is increased in NSCLC and stratifies response.
a,b, Kaplan-Meier curves of patient survival stratified by the ratio in expression between PSME4 and PSME1 for the melanoma cohorts treated with immunotherapy (SKCM ICI, a) or bladder cancer (BLCA ICI, b). Significance determined from Log-ranked test. c, Patients were stratified by PSME1 expression in the ICI cohorts and the response rate for the PSME1-low and PSME1-high groups are shown. PSME1 alone does not consistently categorize a response status among the cancer types analyzed. d, Kaplan-Meier curves of patient survival stratified by the regulatory subunit clusters defined in ‘Fig. 1c’ for the TCGA cohorts. Significance determined from Log-ranked test (n = 9724 tumors). e, H&E staining of tumor or adjacent tissue from 2 representative patients (Scale bar represent 2000 µm.). f, Immunohistochemistry staining for PSME4 of tumor or adjacent tissue from 3 representative patients (Scale bar represent 2000 µm (X0.5), 100 µm (X10) and 20 µm (X40)). g, Immunoblotting band intensity across tumor or adjacent tissues were quantified for PSME4 and normalized to actin as a loading control (two-sided paired student’s t-test *P = 0.0437, n = 5 patients). h, Immunoblotting band intensity across tumor or adjacent lung tissues from an independent cohort were quantified for PSME4 and normalized to actin as a loading control (two-sided paired student’s t-test **P = 0.01, n = 6 patients).
Extended Data Fig. 3 PSME4 is not strongly associated with other factors in Lung Adenocarcinoma.
a – d, Using the protein abundance of PSME4 normalized to the mean abundance of the core proteasome from the CPTAC LUAD cohort compared to patient data, we examined the association to other factors. (a) The significance of the association between each of the factors listed and the abundance of PSME4 across the samples. For discreet factors, the mean abundance between the different groups was compared with a one-way ANOVA. For continuous factors, the significance of the spearman correlation between the protein abundance and factor is displayed. (b) Slight increase in PSME4 abundance in tumors that do not have a KRAS mutation (two-sided student’s t test, n = 111 tumors). (c) Change in abundance of all the proteasome subunits between KRAS mutant and wild type KRAS tumors. As most proteasome subunits are decreased in abundance in KRAS mutant cancers, we conclude that the change we observe in PSME4 is not due specifically to PSME4 level or function. Significance determined from two-sided student’s T test, n = 111 tumors. (d) The abundance of PSME4 normalized to the core in each of the histological subtypes of PSME4 (n = 111 tumors). Variation between the subtypes only occurs in rare groups that cannot clearly be distinguished due to sample size. e-i, Quantification of PSME4 in NSCLC subtypes lung adenocarcinoma (LUAD) and squamous cell lung carcinoma (SQCLC) measured by immunohistochemistry staining. Samples are stratified by subtype (e), smoking level (f), T stage (g), N stage (h) or TNM stage (i). Dots are colored by subtype (LUAD – yellow, SQCLC - red). 50 independent patient samples were assessed. Box plots span the first to third quartiles. Significance determined by Wilcoxon rank sum test.
Extended Data Fig. 4 PSME4 low tumors are enriched in T cell pathways with proteomics but not transcriptomics.
a – c, Pathway enrichment analysis was performed for the tumors in the CPTAC-LUAD cohort that are defined as PSME4 enriched (based on Fig. 1) using the (a) KEGG (b) BIOCARTA or (c) Gene Ontology datasets. The Normalized Enrichment score (for the PSME4-low tumors compared to the PSME4-high tumors) is plotted with the circle size indicated pathway size and the color indicating the significance of the enrichment determined by FDR corrected q-value (n = 111 tumors). d, qPCR of PSME4 in A549 cell line following depletion of PSME4 with shA223 or shA073 compared to shCtrl with and without stimulation with TNFα and IFNγ (T + I) (two-sided paired student’s T test, P values in source data.; n = 3 independent biological experiments; bars indicate mean ± s.d.). e, Lysates of A549 cells with PSME4 knockdown (shA223 and shA073) or control (shCtrl) were blotted for PSME4 and β-Actin as a loading control. The experiment was repeated twice with similar results. f, Quantification of PSME4 band intensity in A549 cell line with PSME4 KD (A223 or A073) or shCtrl (Ctrl) across three independent samples normalized to actin as a loading control and to shCtrl (Welch’s corrected two-sided student’s T-test *P = 0.0186; ***P = 0.0005; bars indicate mean ± s.d.). g, The fold change in gene expression between the A549 cell line following depletion of PSME4 with shA223 compared to shCtrl is plotted against the significance of the change. Genes which passed the FDR adjusted P value cutoff of 0.05 are presented. Significance is determined by Wald test with BH correction.
Extended Data Fig. 5 Proteome and Degradome landscapes classify tumor and adjacent tissues across patients.
a,b, Pairwise Pearson correlation between the proteins identified in each sample by MAPP (a) or the whole cell proteome (b; n = 8 adjacent and 8 tumor samples). c,d, Principal component analysis based on the identities and abundances of the proteins identified by MAPP (c) or whole cell proteome (d). Tumor (T) and adjacent (A) samples are annotated and plotted with principal component PC1 against PC2 (n = 8 adjacent and 8 tumor samples). e, The abundance of proteins that were different between tumor and adjacent lung tissues as determined by MAPP are shown in four datasets: MAPP (n = 16 samples), whole cell Proteomics (n = 16 samples), CPTAC proteomics (n = 215 samples) and TCGA LUAD (c = 573 samples). Proteins not identified in a dataset are shown as grey, otherwise the normalized abundance / expression is shown as a red to blue scale. f, The fold change in abundance for each protein between the tumor and adjacent tissue in the whole cell proteome is plotted against the significance of their difference (negative log10 transformed P value) in grey. The proteins identified as differential in MAPP (listed in table S2) are annotated in red. g, Proteins identified in MAPP organized by their annotated cellular localization (Human Protein Atlas). Proteins are colored based on the mean of degradation ratios between tumor and adjacent tissues across patients (orange: above median degradation ratio, blue: degradation ratio below 0, black: ratio between median and 0). Proteins that are annotated to localize at more than one organelle appear more than once. h,i, The mean ratio of degradation (MAPP) between the tumor and adjacent tissues for proteins annotated to the nucleus (h) or cytosol (i) versus other proteins. The nuclear proteins on average had significantly higher ratio compared to the background proteins (Wilcoxon rank sum test p = 0.037; n = 337 proteins identified across 8 tumor and 8 adjacent tumor samples). Box plots span the first to third quartiles and whiskers show 1.5× interquartile range.
Extended Data Fig. 6 PSME4 is incorporated into multiple species of proteasome complex in multiple localizations.
a,b, Cytosolic and nuclear cellular fractions of A549 were stained with Coomassie (a) and immunoblotted for PSME4 (b). GAPDH and Histone H3 were used as cytosolic and nuclear markers respectively. c, Proteasome complexes were immunoprecipitated (IP) with PSMA1 from A549 cells (with PSME4 depletion or control) that were either treated with TNFα and IFNγ or left untreated and blotted for the indicated proteasome subunits. This experiment was repeated twice with similar results. d,e, Abundance of the proteasome subunits following mass spectrometry analysis of the αPSMA1 immunoprecipitate from nuclear and cytosolic fractions. A heatmap of abundances where values are scaled by row (d). A volcano plot showing the log2 transformed fold change between median abundance of each subunit in the nuclear and cytosolic proteasomes is plotted against the significance of the difference (two-sided student’s T.test; e). Colors indicate the identity of the proteasome subunits. f, The carboxy terminal residue of peptides was used to classify these peptides based on the proteasome activity attributed to their cleavage. The abundance of PSME4 in the samples based on whole cell proteomics correlated with the chymotryptic-like signature (spearman rho = 0.33, n = 8 tumor and 8 adjacent samples). g, Workflow of the size exclusion separation. A549 cells were treated with TNFα and IFNγ (TI) for 24 hours or left untreated, lysed and then recombinant PSME4 was added to the TI treated A549 lysates. h, Lysates were separated by size using Superose6 gel filtration column and blotted against different proteasome subunits as indicated. i, Input lysates of A549 cells treated with TNFα and IFNγ (TI) or untreated used for immunoprecipitation shown in Fig. 3f blotted with the indicated antibody. j,k, Input lysates of A549 cells treated with TNFα and IFNγ (TI) or untreated (j) and the immunoprecipitation with the indicated antibody (k) blotted for the indicated proteasome subunit. Experiments in h-k were repeated twice with similar results.
Extended Data Fig. 7 PSME4 modulates proteasome activity and HLA maturation.
a-c, Proteasome activity assays using fluorogenic substrates LLE-bNA (caspase, β1;a), nLPnLD-AMC (caspase, β1;b), or LLVY-AMC (chymotryptic, β5;c) for 3.5 hours. Relative fluorescence unit (RFU) of the substrate is shown across the 3.5 hours of the experiment (left) or at the endpoint (right). Recombinant PSME4 in different ratios, as indicated, was added to A549 lysates (one-way ANOVA; **P = 0.0022, **** P < 0.0001; bars indicate mean ± s.d.; n = 3 independent samples). d-h, Proteasome activity assays using the nLPnLD-AMC (caspase, β1; d), RLR-AMC (tryptic, β2/ β2i; e), PAL-AMC (chymotryptic, β1i; f), LLVY-AMC (chymotryptic, β5/ β5i; g) or ANW-AMC (chymotryptic, β5i; h) substrates. Relative fluorescence unit (RFU) of the substrate is shown across the 3.5 hours of the experiment (left) or at the endpoint (right). A549 lysates were treated with TNFα and IFNγ (T + I; red) or untreated (UT; black) and recombinant PSME4 was added to the lysate where indicated (two-sided paired student’s T-test) Red squares indicate the portion of the Figure reproduced in Fig. 3 (n = 4 independent samples; bars indicate mean ± s.d.). i, The MFI of HLA on the cell surface was monitored using flow cytometry following acid stripping. PSME4 depletion (shPSME4) increases levels of HLA on the cell surface starting from 2 hours after stripping (2-way-ANOVA ****P ≤ 0.0001, n = 3 independent samples; bars indicate mean ± s.d.). j, The percentage of HLA-high cells was monitored using flow cytometry following acid stripping. PSME4 overexpression (PSME4 OE) decreases levels of HLA on the cell surface starting from 4 hours after stripping. (2-way-ANOVA **P = 0.0033, n = 3 independent samples; bars indicate mean ± s.d.). k,l, The percent of cells with high levels of HLA on the surface is significantly decreased following PSME4 overexpression (k; n = 3 independent samples per condition). By contrast, the intracellular levels of HLA are significantly increased upon PSME4 overexpression (l; bars indicate mean ± s.d.).
Extended Data Fig. 8 The cellular immunopeptidome is altered by PSME4 modulation.
a, The number of peptides identified in A549 cells 6 hours after acid stripping and stimulation with TNFα and IFNγ. Peptide count is shown both for cells depleted of PSME4 (KD) or control (Ctrl). Peptides were derived from n = 3 independent samples per treatment (Wilcoxon rank sum test; bars indicate mean ± s.d.). b, Principal component analysis (PCA) of the peptides identified and their abundances in the immunopeptidomics experiment (n = 3 independent samples). c, The mean fold change ratio between PSME4 depleted (KD) and control (WT) peptides is plotted for all the peptides identified. (One-sided T test of FC versus mu = 0) d, Whole cell proteomics was performed and a volcano plot for the change in protein abundance between the depleted (KD) and control (WT) conditions is shown (two-sided Student’s T test). e, Peptides are divided based on predicted haplotype and the fold change between PSME4 depletion (KD) is shown for each group (n = 3 independent samples). Box plots span the first to third quartiles and whiskers show 1.5× interquartile range. f, The fold change between KD and WT for the 179 peptides which end in K (orange line) was compared to 179 peptides randomly selected from the immunopeptidome 10,000 times (grey). g, A549 cells transfected with a PSME4-expressing plasmid or empty vector as a control. Cell lysates were blotted for PSME4. β-Actin was blotted as a loading control. Experiment was repeated twice with similar results h, Quantification of PSME4 band intensity in A549 cell line with PSME4 OE or Ctrl across n = 3 independent samples normalized to actin as a loading control (two-sided paired student’s t-test **P = 0.0045). i, Principal component analysis (PCA) of the peptides identified and their abundances in the immunopeptidomics experiment. j, Following ratio normalization to control for batch effect, the correlation between the ratios for the 463 altered peptides is shown across the replicates. k, The mean fold change ratio between overexpression (OE) and control peptides is plotted for the 463 peptides differentially presented upon PSME4 overexpression. l, The percentage of peptides with each indicated carboxy terminus is plotted for the peptides significantly increased in the PSME4 overexpression or empty vector control (denoted WT). m, The ratio between the enrichment score for the cellular component groups enriched in peptides increased in expression upon PSME4 overexpression (OE) over control (WT).
Extended Data Fig. 9 PSME4 depletion in KP1.9 cells increases MHC levels.
a, Lysates of KP1.9 cells with PSME4 knockdown (shK369 and shK428, shK569 or shK813) or control (shRFP) were blotted for PSME4 and β-Actin as a loading control. b, Quantification of PSME4 band intensity in KP1.9 cell line with PSME4 KD or Ctrl (shRFP) across independent samples per condition normalized to actin as a loading control and to shRFP (bars indicate mean ± s.d.; two-sided student’s T test, shK428 P = 0.018, shK569 P = 0.0054 or shK813 P = 0.0368). c, KP1.9 cells and healthy mouse lung tissue were blotted for PSME4. β-Actin was blotted as a loading control. d, qPCR shows the expression of PSME4 in KP1.9 cells transfected with a PSME4 overexpression plasmid (n = 3 independent experiments; bars indicate mean ± s.d.). e, KP1.9 cells transfected with a PSME4 overexpression plasmid (+) or GFP (-) as a control. Cell lysates were blotted for PSME4 or PSMA1-7. β-Actin was blotted as a loading control. f, Band intensities of e were quantified for PSME4 and normalized to actin as a loading control (two-sided paired student’s t-test *P = 0.0331; n = 3 independent samples). g, Median fluorescence intensity from flow cytometry analysis of MHC-I expression using a Kb or Db antibody on KP1.9 cells with PSME4 overexpression or control (n = 3 independent samples). Box plots span the first to third quartiles and whiskers show 1.5× interquartile range (Wilcox test). h,i, GO-term enrichment (of key markers from the plasmacytoid DC (h) or mature DCs enriched in immunoregulatory molecules (mregDCs; i) population. Significance determined by FDR corrected q-value.
Extended Data Fig. 10 PSME4 overexpression in KP1.9 cells increases tumor burden in an immune-dependent manner.
a, Weights of C57/B6 mice bearing orthotopic wild type (KP1.9; n = 7), PSME4-overexpressing (OE; n = 7), or PSME4-deficient (KD; n = 8) KP1.9 tumors. Weights are normalized to the starting weight of each mouse. Overexpression shows significantly decreased weight as a proxy for increased disease severity (matched 2-way ANOVA *p = 0.0322). b, Mice bearing PSME4 overexpressing (OE) tumors showed increased tumor burden compared to the control KP1.9 tumors. c, Measurement of the cell growth of KP1.9, KP1.9 expressing shCtrl or shPSME4 (PSME4 KD) for 3 days (n = 3 independent experiments). d, Measurement of the cell growth of KP1.9, KP1.9 expressing GFP overexpression (GFP Ctrl) or PSME4 overexpression (OE) for 3 days (n = 3 independent experiments). e,f, Two representative images per condition in addition to Fig. 6c of H&E staining of lungs from mice bearing KP1.9, KP1.9PSME4 OE, or KP1.9PSME4 KD tumors. g-j, The percentages of the CD45 positive population in the lung (g and h; n = 3 non-inj, 7 KP1.9, 8 KD, 7 OE mice) or spleen (i and j; n = 3 non-inj, 7 KP1.9, 8 KD, 5 OE mice) from the mice bearing KP1.9, KP1.9PSME4 OE, or KP1.9PSME4 KD tumors or mice not injected (non-inj) with tumor cells that are CD4 (g, i) or CD8 (h, j) positive. One way ANOVA with post-hoc TUKEY analysis was used to compare populations (*P ≤ 0.05; bars indicate mean ± s.d.)). k, The percent of different subsets of CD8-positive lymphocytes (naïve, early activated, effector memory [EM] or central memory [CM], which are CD62L and/or CD44 positive, in the lung of mice bearing KP1.9PSME4 OE (n = 5), KP1.9PSME4 KD (n = 8) or KP1.9 (n = 6) tumors compared to mice not bearing tumors (non-inj; n = 2; two-way ANOVA with post-hoc Tukey – P values in Source Data). The portion of the figure marked in the box is reproduced in Fig. 4g (bars indicate mean ± s.d.). l, The body weight of wild-type or immunocompromised RAG1 -/- mice injected with KP1.9 lung tumors expressing either shPSME4 or Ctrl shRNA. The weight of each mouse is normalized to the starting weight at day 1. ‘X’ indicates death.
Supplementary information
Supplementary Information
Supplementary Figs. 1–1.
Supplementary Table 1
Table 1. Antibodies list. Table 2. Primers list. Table 3. Proteomics samples list.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Figs. 2 and 3 and Extended Data Figs. 4, 6, 8 and 9
Unprocessed western blots all figures.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 10
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Javitt, A., Shmueli, M.D., Kramer, M.P. et al. The proteasome regulator PSME4 modulates proteasome activity and antigen diversity to abrogate antitumor immunity in NSCLC. Nat Cancer 4, 629–647 (2023). https://doi.org/10.1038/s43018-023-00557-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-023-00557-4
This article is cited by
-
Cell-autonomous innate immunity by proteasome-derived defence peptides
Nature (2025)
-
Spatial transcriptomics reveals unique metabolic profile and key oncogenic regulators of cervical squamous cell carcinoma
Journal of Translational Medicine (2024)
-
Taking the temperature of lung cancer antigens
Nature Cancer (2023)
-
Protein quality control: from molecular mechanisms to therapeutic intervention—EMBO workshop, May 21–26 2023, Srebreno, Croatia
Cell Stress and Chaperones (2023)